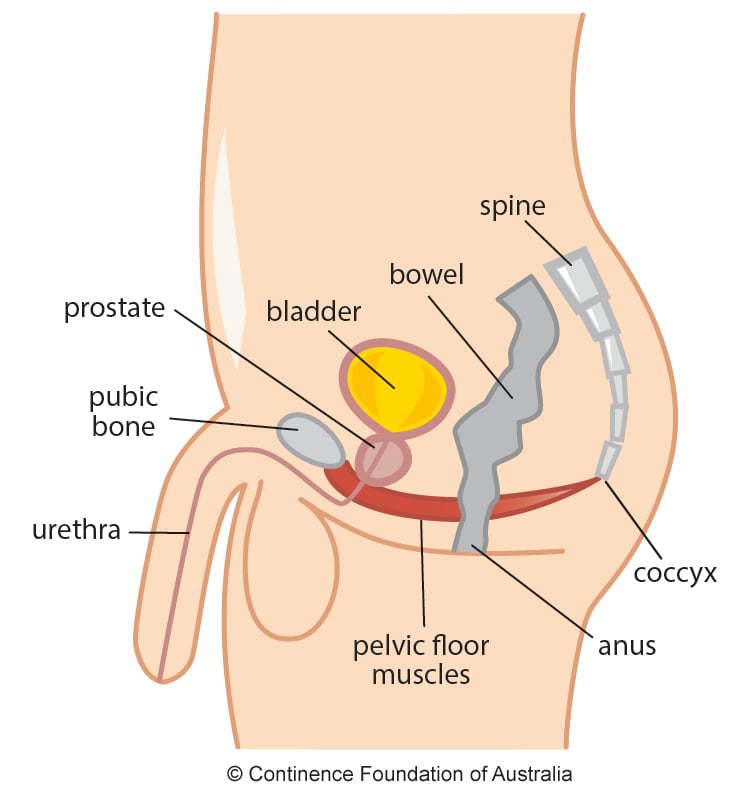
The prostate, a small-sized gland, located at the base of the bladder, can be the site of two distinct processes. The first is a benign growth, called hyperplasia. The second is prostate cancer, which appears associated or not with benign growth and which appears almost always after men turn 50 years old.

Radical prostatectomy, removal of the prostate and seminal vesicles, is the oldest and possibly the most effective method of treating localized prostate cancer. However, this operation causes many complications, among which urinary incontinence is the most distressing.

The International Continence Society (ICS) defines urinary incontinence as a complaint of any leakage (involuntary leakage) of urine. In men, it can occur mainly after the treatment of benign prostatic hyperplasia and the treatment of prostate cancer.
The frequency of urinary incontinence varies depending on the type of surgery, surgical technique, patient age and health conditions, but tends to improve after one to two years. However, some patients remain with urinary incontinence. It has been shown in urodynamic studies high frequencies (87%) of incontinence in patients after radical prostatectomy.
Why does urine leakage happen?
The sphincter mechanisms can be divided into a proximal and a distal component.
During a prostatectomy for benign disease, the proximal sphincter is always injured, and continence is dependent on the distal component. In radical prostatectomy, the the proximal sphincter is almost completely resected with the specimen, as well as the proximal portions of the distal sphincter. In this case, continence will be exclusively dependent on the distal part of the distal urethral sphincter, where there are voluntary muscle fibers, which can be consciously contracted. The external sphincter is important in continence during sudden increases in intra-abdominal pressure (exertion).

Risk Factors
- advanced age
- intraoperative blood loss
- prostate volume
- previous endoscopic prostatic resection
- previous radiotherapy
- preservation of nerve bundles and the bladder neck
Treatment
Functional pelvic floor training guided by a pelvic floor physiotherapist is one of the gold standard treatments a method that works with specific pelvic floor contraction aimed at improving the effectiveness of the external urethral sphincter during periods of increased intra-abdominal pressure.
We can use specific techniques, such as “biofeedback”; functional electrical stimulation of the pelvic floor muscles with electrodes; transcutaneous electrical stimulation or a combination of these methods, bladder control techniques. Conservative treatment should be combined with lifestyle changes and modifications, such as decreasing or eliminating caffeine and smoking.
Do you have any questions? Get in touch and I will be happy to help you.

